Infectious diseases, vaccines and treatments
Session: Poster Session A
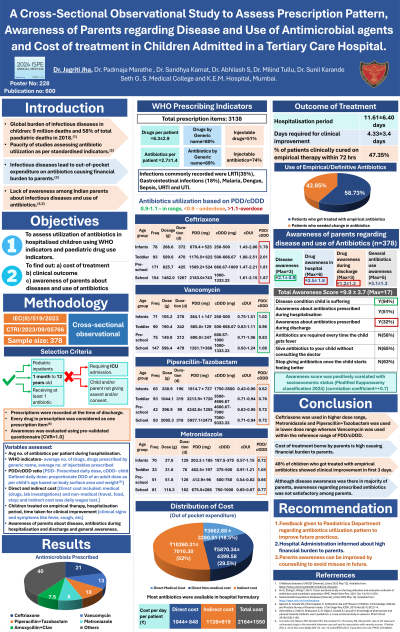
(228) A Cross-Sectional Observational Study to Assess Prescription Pattern, Awareness of Parents regarding Disease and Use of Antimicrobial agents and Cost of treatment in Children Admitted in a Tertiary Care Hospital.
Monday, August 26, 2024
8:00 AM - 6:00 PM CEST
Location: Convention Hall II
.jpg)
Jagriti Pankaj Jha, MBBS, MD Pharmacology (she/her/hers)
Junior Resident
Seth G.S. Medical College and K.E.M. Hospital
Mumbai, India
Presenting Author(s)
Background: Infectious diseases in children caused 9 million deaths worldwide and 58% of pediatric deaths in 2018. Keeping in view the paucity of pediatric studies in India assessing antibiotic utilization as per standardized indicators, lack of parental awareness, and high out of pocket expenditure on antibiotics causing financial burden, this study was planned with the following objectives:
Objectives: 1. To analyse prescription pattern of antibiotics in hospitalised children using WHO indicators and paediatric drug use indicators. 2. To find out awareness of parents, cost of treatment and clinical outcome of infection.
Methods: A cross-sectional observational study [IEC(II)/519/2023; CTRI/2023/09/057669] in 368 hospitalized children (1 month to 12 years of age) receiving antibiotics is being conducted at a tertiary care hospital. Variables assessed: average number of drugs/ prescription, Prescribed daily dose (PDD), Child Defined Daily Dose (cDDD), PDD/cDDD ratio, Child Drug Utilization Index (cDUI), awareness of parents using a pre-validated questionnaire (CVR-1.0), treatment cost analysis and treatment outcome (empirical antibiotics, time taken for cure). Statistical analysis has been done using descriptive statistics.
Results: • Number of drugs prescribed was 8.85±3.34 per child. Antibiotics prescribed per child was 2.8±1.4. Ceftriaxone (22%), Vancomycin (13%), Metronidazole (11%), Piperacillin + Tazobactam (11%) and Cefotaxime(5.8%) were commonly prescribed. • cDUI of Ceftriaxone was higher than reference range across all age groups [Infants (1.08-2.16), pre-school children (1.30-1.49), toddlers (1.83-2.04) and school going children (1.46-1.94)]. cDUI of Vancomycin was in range for toddlers (0.83-1.19) and school going children (0.93-1.04). While cDUI of Piperacillin-tazobactam and Metronidazole was lower than reference range for all the age groups. • 95.52% parents knew about the disease (2.82±0.88, total score-4), however awareness about the drugs prescribed during hospitalization and at discharge were 3.47±1.81 (total score-6) and 1.25±1.28 (total score-3) respectively. General awareness about use of antibiotics was inadequate. • Average direct and indirect cost were ₹13159.41±8733.62 and ₹10133.58±9242.45 per child respectively. • Clinical improvement was seen in 6.88±4.33 days with 12.64±6.69 days of hospitalization and 53% children improved with empirical therapy out of which 75% improved in first 96 hours.
Conclusions: Ceftriaxone was used in higher while Piperacillin-tazobactam and Metronidazole were used in lower dose range. Vancomycin was used within reference dose range. Awareness about the use of antibiotics was suboptimal.
Co-authors: Dr Padmaja Marathe, Dr Sandhya Kamat, Dr Milind Tullu, Dr Sunil Karande, Dr Abhilash S
Objectives: 1. To analyse prescription pattern of antibiotics in hospitalised children using WHO indicators and paediatric drug use indicators. 2. To find out awareness of parents, cost of treatment and clinical outcome of infection.
Methods: A cross-sectional observational study [IEC(II)/519/2023; CTRI/2023/09/057669] in 368 hospitalized children (1 month to 12 years of age) receiving antibiotics is being conducted at a tertiary care hospital. Variables assessed: average number of drugs/ prescription, Prescribed daily dose (PDD), Child Defined Daily Dose (cDDD), PDD/cDDD ratio, Child Drug Utilization Index (cDUI), awareness of parents using a pre-validated questionnaire (CVR-1.0), treatment cost analysis and treatment outcome (empirical antibiotics, time taken for cure). Statistical analysis has been done using descriptive statistics.
Results: • Number of drugs prescribed was 8.85±3.34 per child. Antibiotics prescribed per child was 2.8±1.4. Ceftriaxone (22%), Vancomycin (13%), Metronidazole (11%), Piperacillin + Tazobactam (11%) and Cefotaxime(5.8%) were commonly prescribed. • cDUI of Ceftriaxone was higher than reference range across all age groups [Infants (1.08-2.16), pre-school children (1.30-1.49), toddlers (1.83-2.04) and school going children (1.46-1.94)]. cDUI of Vancomycin was in range for toddlers (0.83-1.19) and school going children (0.93-1.04). While cDUI of Piperacillin-tazobactam and Metronidazole was lower than reference range for all the age groups. • 95.52% parents knew about the disease (2.82±0.88, total score-4), however awareness about the drugs prescribed during hospitalization and at discharge were 3.47±1.81 (total score-6) and 1.25±1.28 (total score-3) respectively. General awareness about use of antibiotics was inadequate. • Average direct and indirect cost were ₹13159.41±8733.62 and ₹10133.58±9242.45 per child respectively. • Clinical improvement was seen in 6.88±4.33 days with 12.64±6.69 days of hospitalization and 53% children improved with empirical therapy out of which 75% improved in first 96 hours.
Conclusions: Ceftriaxone was used in higher while Piperacillin-tazobactam and Metronidazole were used in lower dose range. Vancomycin was used within reference dose range. Awareness about the use of antibiotics was suboptimal.
Co-authors: Dr Padmaja Marathe, Dr Sandhya Kamat, Dr Milind Tullu, Dr Sunil Karande, Dr Abhilash S
