Rare diseases
Session: Poster Session C
(304) Healthcare resource utilization among patients with multiple system atrophy in US claims database
Wednesday, August 28, 2024
8:00 AM - 1:30 PM CEST
Location: Convention Hall II
- SK
Sigal Kaplan, PhD, BPharm
Director of Epidemiology
Teva Pharmaceutical Industries Ltd, Israel., Israel - HX
Handing Xie
Teva, United States
- AK
Amit Kumar
KMK Consulting, Inc, United States
Presenting Author(s)
Co-Author(s)
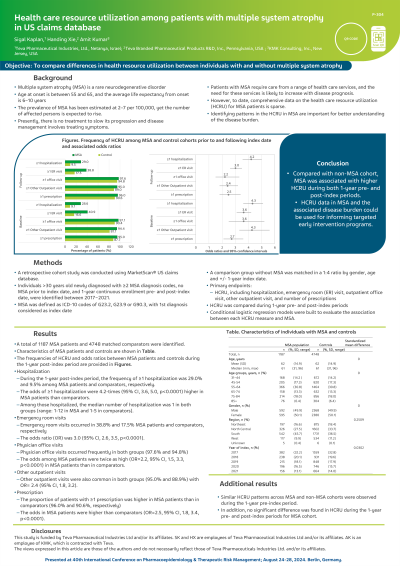
Background: MSA is a rare neurodegenerative disorder, yet the number of affected persons is expected to rise. Presently, there is no treatment to slow its progression and disease management involves treating symptoms. Data on HCRU for MSA is sparse. Identifying patterns in the HCRU in MSA are important for better understanding of the disease burden.
Objectives: To compare differences in health resource utilization (HCRU) between individuals with and without multiple system atrophy (MSA)
Methods: A retrospective cohort study was conducted using MarketScan® US claims database. Individuals >30 years old newly diagnosed with ≥2 MSA diagnosis codes (defined as ICD-10 codes of G23.2, G23.9 or G90.3, with 1st diagnosis considered as index date), no MSA prior to index date, and 1-year continuous enrollment pre- and post-index date, were identified between 2017−2021. A comparison group without MSA was matched in a 1:4 ratio by gender, age and +/- 1-year index date. HCRU was compared between two groups during 1-year pre- and post-index periods. Conditional logistic regression models were built to evaluate the association between each HCRU measure and MSA.
Results: A total of 1187 MSA patients and 4748 matched comparators were identified.
During the 1-year post-index period, the frequency of ≥1 hospitalization was 29.0% and 9.5% among MSA patients and comparators, respectively. The odds of ≥1 hospitalization were 4.2-times (95% CI, 3.6, 5.0, p< 0.0001) higher in MSA patients than comparators. Among those hospitalized, the median number of hospitalizations was 1 in both groups (range: 1-12 in MSA and 1-5 in comparators). Emergency room visits occurred in 38.8% and 17.5% MSA patients and comparators, respectively and the odds ratio (OR) was 3.0 (95% CI, 2.6, 3.5, p< 0.0001).
Physician office visits occurred frequently in both groups (97.6% and 94.8%), but the odds among MSA patients were twice as high (OR=2.2, 95% CI, 1.5, 3.3, p< 0.0001) in MSA patients than in comparators.
Other outpatient visits were also common in both groups (95.0% and 88.9%) with OR= 2.4 (95% CI, 1.8, 3.2). The proportion of patients with ≥1 prescription was higher in MSA patients than in comparators (96.0% and 90.6%, respectively) with higher odds in MSA patients than comparators (OR=2.5, 95% CI, 1.8, 3.4, p< 0.0001).
Similar HCRU patterns across MSA and non-MSA cohorts were observed during the 1-year pre-index period. In addition, no significant difference was found in HCRU during the 1-year pre- and post-index periods for MSA cohort.
Conclusions: Compared with non-MSA cohort, MSA was associated with higher HCRU during both 1-year pre- and post-index periods. HCRU data in MSA and the associated disease burden could be used for informing targeted early intervention programs.
Objectives: To compare differences in health resource utilization (HCRU) between individuals with and without multiple system atrophy (MSA)
Methods: A retrospective cohort study was conducted using MarketScan® US claims database. Individuals >30 years old newly diagnosed with ≥2 MSA diagnosis codes (defined as ICD-10 codes of G23.2, G23.9 or G90.3, with 1st diagnosis considered as index date), no MSA prior to index date, and 1-year continuous enrollment pre- and post-index date, were identified between 2017−2021. A comparison group without MSA was matched in a 1:4 ratio by gender, age and +/- 1-year index date. HCRU was compared between two groups during 1-year pre- and post-index periods. Conditional logistic regression models were built to evaluate the association between each HCRU measure and MSA.
Results: A total of 1187 MSA patients and 4748 matched comparators were identified.
During the 1-year post-index period, the frequency of ≥1 hospitalization was 29.0% and 9.5% among MSA patients and comparators, respectively. The odds of ≥1 hospitalization were 4.2-times (95% CI, 3.6, 5.0, p< 0.0001) higher in MSA patients than comparators. Among those hospitalized, the median number of hospitalizations was 1 in both groups (range: 1-12 in MSA and 1-5 in comparators). Emergency room visits occurred in 38.8% and 17.5% MSA patients and comparators, respectively and the odds ratio (OR) was 3.0 (95% CI, 2.6, 3.5, p< 0.0001).
Physician office visits occurred frequently in both groups (97.6% and 94.8%), but the odds among MSA patients were twice as high (OR=2.2, 95% CI, 1.5, 3.3, p< 0.0001) in MSA patients than in comparators.
Other outpatient visits were also common in both groups (95.0% and 88.9%) with OR= 2.4 (95% CI, 1.8, 3.2). The proportion of patients with ≥1 prescription was higher in MSA patients than in comparators (96.0% and 90.6%, respectively) with higher odds in MSA patients than comparators (OR=2.5, 95% CI, 1.8, 3.4, p< 0.0001).
Similar HCRU patterns across MSA and non-MSA cohorts were observed during the 1-year pre-index period. In addition, no significant difference was found in HCRU during the 1-year pre- and post-index periods for MSA cohort.
Conclusions: Compared with non-MSA cohort, MSA was associated with higher HCRU during both 1-year pre- and post-index periods. HCRU data in MSA and the associated disease burden could be used for informing targeted early intervention programs.
