Pregnancy and lactation
Session: Poster Session B
(307) Replicating a Published Real-World Evidence Study to Analyze Maternal Delivery Complications Using Electronic Medical Records from Community Hospitals
Tuesday, August 27, 2024
8:00 AM - 6:00 PM CEST
Location: Convention Hall II
- HB
Hannah Borda
Costello Medical, United States
- AZ
Anna Zolotor
Costello Medical, United States
- AA
Audrey Artignan
Costello Medical, United Kingdom
- AB
Amy Buchanan-Hughes
Costello Medical, United States
Presenting Author(s)
Co-Author(s)
Background
Real-world data (RWD) in the US are often sourced from employer-sponsored insurance plans or major provider networks, leading to underrepresentation of patients with lower socioeconomic status. InsightsDB, from the Institute for Health Metrics, collates electronic health record (EHR) data from ~100 community hospitals across 30 states with linkage to social determinants of health (SDOH) for over 5 million unique patients.
Objectives
To explore the strengths and limitations of insightsDB by replicating aspects of a published study (Huennekens 2020; DOI: 10.1016/j.jcjq.2020.08.007) conducted in a large Illinois health system’s EHR depository.
Methods
We conducted a retrospective cohort study using the insightsDB database, identifying all deliveries from January 2017–June 2023 using the International Classification of Diseases, Tenth Revision (ICD-10) codes. The primary outcome was the presence of hemorrhagic, infectious, operative, or thrombotic maternal delivery complications. We evaluated association with demographic traits, comorbidities, and delivery characteristics using multivariable logistic regression. Where methodologically feasible, we compared our results to those reported in Huennekens 2020.
Results
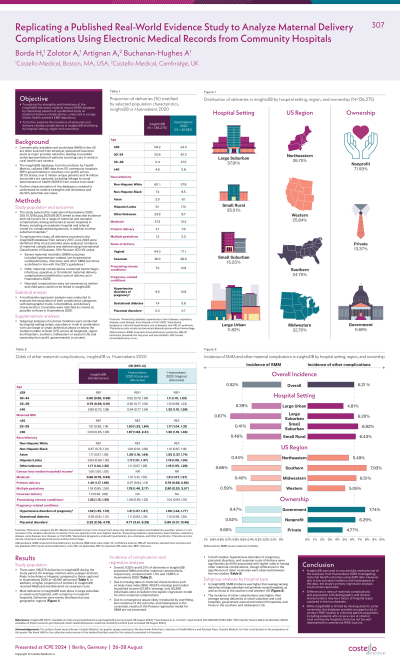
In the primary analysis, 136,275 mothers in the insightsDB population delivered children during the study period, with an overall incidence of maternal complications of 6.2%. Due to missing data on maternal characteristics, 50,358 individuals were included in our regression model. In both studies, hypertensive disorders of pregnancy, placental disorders, and cesarean route of delivery were significantly (p < 0.05) associated with higher odds of having a delivery complication. Preexisting chronic conditions (OR 1.32; 95% CI 1.15-1.51) and preterm deliveries (OR 1.43; 95% CI 1.20-1.70) were associated with complications in insightsDB, but not in Huennekens 2020; most levels of higher maternal BMI and race or ethnicity were significant in Huennekens 2020, but not in InsightsDB.
Conclusions
Our study of community hospital patients had a lower rate of complications than that recorded in Huennekens 2020, in which a majority of deliveries took place in academic and specialist medical centers, where women with high-risk pregnancies would be referred. Conversely, the greater increase in risk of complications in deliveries with pre-existing chronic conditions or preterm birth in the insightsDB population may be due to challenges with managing these scenarios in less well-resourced hospital settings.
Real-world data (RWD) in the US are often sourced from employer-sponsored insurance plans or major provider networks, leading to underrepresentation of patients with lower socioeconomic status. InsightsDB, from the Institute for Health Metrics, collates electronic health record (EHR) data from ~100 community hospitals across 30 states with linkage to social determinants of health (SDOH) for over 5 million unique patients.
Objectives
To explore the strengths and limitations of insightsDB by replicating aspects of a published study (Huennekens 2020; DOI: 10.1016/j.jcjq.2020.08.007) conducted in a large Illinois health system’s EHR depository.
Methods
We conducted a retrospective cohort study using the insightsDB database, identifying all deliveries from January 2017–June 2023 using the International Classification of Diseases, Tenth Revision (ICD-10) codes. The primary outcome was the presence of hemorrhagic, infectious, operative, or thrombotic maternal delivery complications. We evaluated association with demographic traits, comorbidities, and delivery characteristics using multivariable logistic regression. Where methodologically feasible, we compared our results to those reported in Huennekens 2020.
Results
In the primary analysis, 136,275 mothers in the insightsDB population delivered children during the study period, with an overall incidence of maternal complications of 6.2%. Due to missing data on maternal characteristics, 50,358 individuals were included in our regression model. In both studies, hypertensive disorders of pregnancy, placental disorders, and cesarean route of delivery were significantly (p < 0.05) associated with higher odds of having a delivery complication. Preexisting chronic conditions (OR 1.32; 95% CI 1.15-1.51) and preterm deliveries (OR 1.43; 95% CI 1.20-1.70) were associated with complications in insightsDB, but not in Huennekens 2020; most levels of higher maternal BMI and race or ethnicity were significant in Huennekens 2020, but not in InsightsDB.
Conclusions
Our study of community hospital patients had a lower rate of complications than that recorded in Huennekens 2020, in which a majority of deliveries took place in academic and specialist medical centers, where women with high-risk pregnancies would be referred. Conversely, the greater increase in risk of complications in deliveries with pre-existing chronic conditions or preterm birth in the insightsDB population may be due to challenges with managing these scenarios in less well-resourced hospital settings.
