GLP-1 receptor agonists
Session: Poster Session C
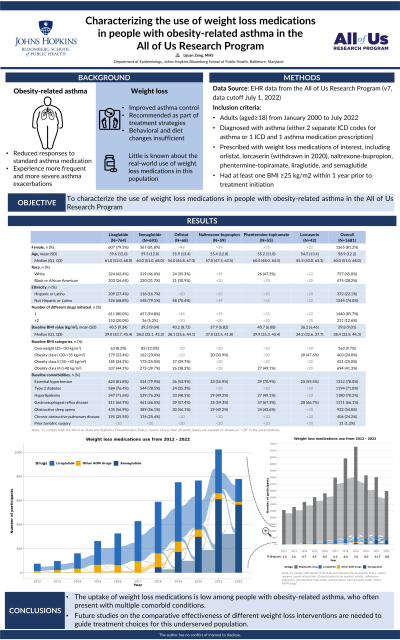
(091) Characterizing the use of weight loss medications in people with obesity-related asthma in the All of Us Research Program
Wednesday, August 28, 2024
8:00 AM - 1:30 PM CEST
Location: Convention Hall II
Lijuan Zeng, MHS (she/her/hers)
PhD Candidate
Johns Hopkins Bloomberg School of Public Health, United States
Presenting Author(s)
Background: People with obesity-related asthma have reduced responses to standard asthma medications and experience more frequent and more severe asthma exacerbations. Weight loss is associated with improved asthma control, and current asthma management guidelines recommend incorporating weight loss as part of treatment strategies. However, little is known about the real-world use of weight loss medications in people with asthma.
Objectives: This study aims to characterize the use of weight loss medications in people with obesity-related asthma.
Methods: A retrospective cohort study was conducted using electronic medical record data from the All of Us Research Program (v7, data cutoff July 1, 2022). The study population comprised adults (aged 18 and older) diagnosed with asthma who were prescribed weight loss medications and had at least one measurement of body mass index (BMI) greater than or equal to 25 kg/m2 within a year preceding treatment initiation. Asthma condition was ascertained through either i) two separate International Classification of Diseases (ICD) codes for asthma or ii) one asthma ICD diagnosis code and one asthma medication prescription. The weight loss medications of interest in this study included orlistat, naltrexone-bupropion, phentermine-topiramate, liraglutide, semaglutide, and lorcaserin (withdrawn in 2020). Descriptive statistics were used to summarize population characteristics, comorbidities, and concomitant medication uses. Changes in weight loss medications over time were visualized using Sankey diagrams.
Results: Out of 39,155 participants with asthma and obesity/overweight, 1681 (4.3%) were prescribed the weight loss medications of interest between 2008 and 2022. Liraglutide was the most-prescribed first medication (n=764), followed by semaglutide (n=693), orlistat (n=68), naltrexone-bupropion (n=59), phentermine-topiramate (n=55), and lorcaserin (n=42). The mean age was 58.9 years old (SD: 12.2), with a predominance of female participants (80.8%). The racial composition was 45.0% White and 28.2 % Black or African American. The mean BMI was 39.8 kg/m2 (SD: 9.0). Notable comorbidities included essential hypertension (78%), type 2 diabetes (71.0%), hyperlipidemia (70.2%), gastroesophageal reflux disease (66.1%), and obstructive sleep apnea (54.8%). About 15% of the population initiated more than two different weight loss medications of interest during the follow-up.
Conclusions: The uptake of weight loss medications is low among people with obesity-related asthma, who often present with multiple comorbid conditions. Future studies on the comparative effectiveness of different weight loss interventions are needed to guide treatment choices for this underserved population.
Objectives: This study aims to characterize the use of weight loss medications in people with obesity-related asthma.
Methods: A retrospective cohort study was conducted using electronic medical record data from the All of Us Research Program (v7, data cutoff July 1, 2022). The study population comprised adults (aged 18 and older) diagnosed with asthma who were prescribed weight loss medications and had at least one measurement of body mass index (BMI) greater than or equal to 25 kg/m2 within a year preceding treatment initiation. Asthma condition was ascertained through either i) two separate International Classification of Diseases (ICD) codes for asthma or ii) one asthma ICD diagnosis code and one asthma medication prescription. The weight loss medications of interest in this study included orlistat, naltrexone-bupropion, phentermine-topiramate, liraglutide, semaglutide, and lorcaserin (withdrawn in 2020). Descriptive statistics were used to summarize population characteristics, comorbidities, and concomitant medication uses. Changes in weight loss medications over time were visualized using Sankey diagrams.
Results: Out of 39,155 participants with asthma and obesity/overweight, 1681 (4.3%) were prescribed the weight loss medications of interest between 2008 and 2022. Liraglutide was the most-prescribed first medication (n=764), followed by semaglutide (n=693), orlistat (n=68), naltrexone-bupropion (n=59), phentermine-topiramate (n=55), and lorcaserin (n=42). The mean age was 58.9 years old (SD: 12.2), with a predominance of female participants (80.8%). The racial composition was 45.0% White and 28.2 % Black or African American. The mean BMI was 39.8 kg/m2 (SD: 9.0). Notable comorbidities included essential hypertension (78%), type 2 diabetes (71.0%), hyperlipidemia (70.2%), gastroesophageal reflux disease (66.1%), and obstructive sleep apnea (54.8%). About 15% of the population initiated more than two different weight loss medications of interest during the follow-up.
Conclusions: The uptake of weight loss medications is low among people with obesity-related asthma, who often present with multiple comorbid conditions. Future studies on the comparative effectiveness of different weight loss interventions are needed to guide treatment choices for this underserved population.
