Biologics and conditions treated with biologics
Session: Poster Session A
(008) Disease Activity in Rheumatoid Arthritis Patients Initiating Anti-Obesity Medication in a Longitudinal US-Based Real-World Cohort
Monday, August 26, 2024
8:00 AM - 6:00 PM CEST
Location: Convention Hall II
- JP
Jessica R. Probst, MPH (she/her/hers)
Principal, Real World Evidence
OM1, United States - MQ
Meaghan E. Quinn
OM1, United States
Presenting Author(s)
Co-Author(s)
Background: Given the increasing use of anti-obesity medications in managing type II diabetes and obesity, it is important to evaluate their impacts on comorbid conditions. Literature suggests patients with obesity experience differential treatment response and increased disease activity scores.
Objectives: To describe RA burden, using observed and estimated Clinical Disease Activity Index scores, in patients treated with anti-obesity medication in a US real-world cohort.
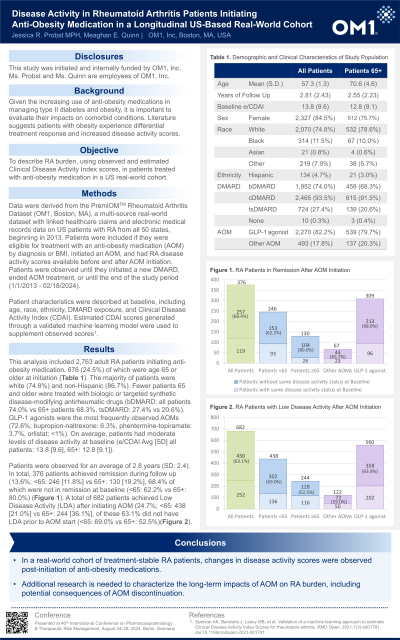
Methods: Data were derived from the PremiOM™ Rheumatoid Arthritis Dataset (OM1, Boston, MA), a multi-source real-world dataset with linked healthcare claims and electronic medical records data on US patients with RA from all 50 states, beginning in 2013. Patients were included if they were eligible for treatment with an anti-obesity medication (AOM) by diagnosis or BMI, initiated an AOM, and had RA disease activity scores available before and after AOM initiation. Patients were observed until they initiated a new DMARD, ended AOM treatment, or until the end of the study period (1/1/2013 - 2/18/2024).
Patient characteristics were described at baseline, including age, race, ethnicity, DMARD exposure, and Clinical Disease Activity Index (CDAI). Estimated CDAI scores generated through a validated machine learning model were used to supplement observed scores (Spencer et al, 2021).
Results: This analysis included 2,763 adult RA patients initiating anti-obesity medication (2,327 women and 512 men), 676 (24.5%) of which were age 65 or older at initiation. The majority of patients were white (74.8%) and non-Hispanic (86.7%). Fewer patients 65 and older were treated with biologic or targeted synthetic disease-modifying antirheumatic drugs (bDMARD: all patients 74.0% vs 65+ patients 68.3%, tsDMARD: 27.4% vs 20.6%). GLP-1 agonists were the most frequently observed AOMs (72.6%; bupropion-naltrexone: 6.3%, phentermine-topiramate: 3.7%, orlistat: <1%). On average, patients had moderate levels of disease activity at baseline (CDAI Avg [SD] all patients: 13.8 [9.6], 65+: 12.8 [9.1]).
Patients were observed for an average of 2.8 years (SD: 2.4). A total of 682 patients achieved Low Disease Activity (LDA) after initiating AOM (24.7%; <65: 438 [21.0%] vs 65+: 244 [36.1%], of these 63.1% did not have LDA prior to AOM start ( <65: 69.0% vs 65+: 52.5%). In total, 376 patients achieved remission during follow up (13.6%; <65: 246 [11.8%] vs 65+: 130 [19.2%], 68.4% of which were not in remission at baseline ( <65: 62.2% vs 65+: 80.0%).
Conclusions: In a real-world cohort of treatment-stable RA patients, changes in disease activity scores were observed post-initiation of anti-obesity medications. Additional research is needed to characterize the long-term impacts of AOM on RA burden, including potential consequences of AOM discontinuation.
Objectives: To describe RA burden, using observed and estimated Clinical Disease Activity Index scores, in patients treated with anti-obesity medication in a US real-world cohort.
Methods: Data were derived from the PremiOM™ Rheumatoid Arthritis Dataset (OM1, Boston, MA), a multi-source real-world dataset with linked healthcare claims and electronic medical records data on US patients with RA from all 50 states, beginning in 2013. Patients were included if they were eligible for treatment with an anti-obesity medication (AOM) by diagnosis or BMI, initiated an AOM, and had RA disease activity scores available before and after AOM initiation. Patients were observed until they initiated a new DMARD, ended AOM treatment, or until the end of the study period (1/1/2013 - 2/18/2024).
Patient characteristics were described at baseline, including age, race, ethnicity, DMARD exposure, and Clinical Disease Activity Index (CDAI). Estimated CDAI scores generated through a validated machine learning model were used to supplement observed scores (Spencer et al, 2021).
Results: This analysis included 2,763 adult RA patients initiating anti-obesity medication (2,327 women and 512 men), 676 (24.5%) of which were age 65 or older at initiation. The majority of patients were white (74.8%) and non-Hispanic (86.7%). Fewer patients 65 and older were treated with biologic or targeted synthetic disease-modifying antirheumatic drugs (bDMARD: all patients 74.0% vs 65+ patients 68.3%, tsDMARD: 27.4% vs 20.6%). GLP-1 agonists were the most frequently observed AOMs (72.6%; bupropion-naltrexone: 6.3%, phentermine-topiramate: 3.7%, orlistat: <1%). On average, patients had moderate levels of disease activity at baseline (CDAI Avg [SD] all patients: 13.8 [9.6], 65+: 12.8 [9.1]).
Patients were observed for an average of 2.8 years (SD: 2.4). A total of 682 patients achieved Low Disease Activity (LDA) after initiating AOM (24.7%; <65: 438 [21.0%] vs 65+: 244 [36.1%], of these 63.1% did not have LDA prior to AOM start ( <65: 69.0% vs 65+: 52.5%). In total, 376 patients achieved remission during follow up (13.6%; <65: 246 [11.8%] vs 65+: 130 [19.2%], 68.4% of which were not in remission at baseline ( <65: 62.2% vs 65+: 80.0%).
Conclusions: In a real-world cohort of treatment-stable RA patients, changes in disease activity scores were observed post-initiation of anti-obesity medications. Additional research is needed to characterize the long-term impacts of AOM on RA burden, including potential consequences of AOM discontinuation.
