Biologics and conditions treated with biologics
Session: Poster Session A
(026) Potential Drug Interaction in Janus Kinase Inhibitors Users Among Patients with Rheumatoid Arthritis or Psoriatic arthritis in Taiwan
Monday, August 26, 2024
8:00 AM - 6:00 PM CEST
Location: Convention Hall II
- YS
Yu-Hsuan Joni SHAO, PhD
Professor
Taipei Medical University, Taiwan (Republic of China) - YC
Yi-Ming Chen
Taichung Veterans General Hospital, Taiwan (Republic of China)
Presenting Author(s)
Co-Author(s)
Background: Target intracellular signaling pathways (Janus kinase [JAK] inhibitors) have been successfully developed and implemented as rheumatoid arthritis (RA) therapies. JAK safety profiles of JAK are generally similar to other biologics, with the exception of an increased incidence of herpes zoster infection and warnings for an increased risk of thromboembolism. However, JAK has unique pharmacokinetic profiles, and subsequently drug interaction profiles.
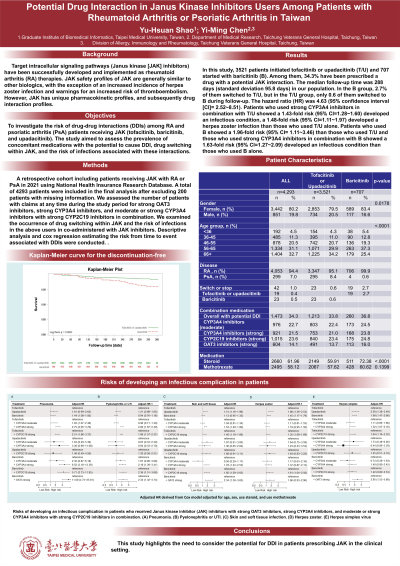
Objectives: To investigate the risk of drug-drug interactions (DDIs) among RA and psoriatic arthritis (PsA) patients receiving JAK (tofacitinib, baricitinib, and upadacitinib). The study aimed to assess the prevalence of concomitant medications with the potential to cause DDI, drug switching within JAK, and the risk of infections associated with these interactions.
Methods: A retrospective cohort including patients receiving JAK with RA or PsA in 2021 using National Health Insurance Research Database. A total of 4293 patients were included in the final analysis after excluding 200 patients with missing information. We assessed the number of patients with claims at any time during the study period for strong OAT3 inhibitors, strong CYP3A4 inhibitors, and moderate or strong CYP3A4 inhibitors with strong CYP2C19 inhibitors in combination. We examined the occurrence of drug switching within JAK and the risk of infections in the above users in co-administered with JAK inhibitors. Descriptive analysis and cox regression estimating the risk from time to event associated with DDIs were conducted.
Results: In this study, 3521 patients initiated tofacitinib or upadacitinib (T/U) and 707 started with baricitinib (B). Among them, 34.3% have been prescribed a drug with a potential JAK interaction. The median follow-up time was 288 days (standard deviation 95.8 days) in our population. In the B group, 2.7% of them switched to T/U, but in the T/U group, only 0.6 of them switched to B during follow-up. The hazard ratio (HR) was 4.63 (95% confidence interval [CI]= 2.52~8.51). Patients who used strong CYP3A4 inhibitors in combination with T/U showed a 1.43-fold risk (95% CI=1.28~1.60) developed an infectious condition, a 1.48-fold risk (95% CI=1.11~1.97) developed a herpes zoster infection than those who used T/U alone. Patients who used B showed a 1.96-fold risk (95% CI= 1.11~3.46) than those who used T/U and those who used strong CYP3A4 inhibitors in combination with B showed a 1.63-fold risk (95% CI=1.27~2.09) developed an infectious condition than those who used B alone.
Conclusions: This study highlights the need to consider the potential for DDI in patients prescribing JAK in the clinical setting.
Objectives: To investigate the risk of drug-drug interactions (DDIs) among RA and psoriatic arthritis (PsA) patients receiving JAK (tofacitinib, baricitinib, and upadacitinib). The study aimed to assess the prevalence of concomitant medications with the potential to cause DDI, drug switching within JAK, and the risk of infections associated with these interactions.
Methods: A retrospective cohort including patients receiving JAK with RA or PsA in 2021 using National Health Insurance Research Database. A total of 4293 patients were included in the final analysis after excluding 200 patients with missing information. We assessed the number of patients with claims at any time during the study period for strong OAT3 inhibitors, strong CYP3A4 inhibitors, and moderate or strong CYP3A4 inhibitors with strong CYP2C19 inhibitors in combination. We examined the occurrence of drug switching within JAK and the risk of infections in the above users in co-administered with JAK inhibitors. Descriptive analysis and cox regression estimating the risk from time to event associated with DDIs were conducted.
Results: In this study, 3521 patients initiated tofacitinib or upadacitinib (T/U) and 707 started with baricitinib (B). Among them, 34.3% have been prescribed a drug with a potential JAK interaction. The median follow-up time was 288 days (standard deviation 95.8 days) in our population. In the B group, 2.7% of them switched to T/U, but in the T/U group, only 0.6 of them switched to B during follow-up. The hazard ratio (HR) was 4.63 (95% confidence interval [CI]= 2.52~8.51). Patients who used strong CYP3A4 inhibitors in combination with T/U showed a 1.43-fold risk (95% CI=1.28~1.60) developed an infectious condition, a 1.48-fold risk (95% CI=1.11~1.97) developed a herpes zoster infection than those who used T/U alone. Patients who used B showed a 1.96-fold risk (95% CI= 1.11~3.46) than those who used T/U and those who used strong CYP3A4 inhibitors in combination with B showed a 1.63-fold risk (95% CI=1.27~2.09) developed an infectious condition than those who used B alone.
Conclusions: This study highlights the need to consider the potential for DDI in patients prescribing JAK in the clinical setting.
