Pregnancy and lactation
Session: Poster Session B
(329) Using Real-World Data to Quantify the Rate of Unintended Pregnancies and Specified Adverse Events in Women Prescribed Oral Levonorgestrel 30µg or Levonorgestrel Implant
Tuesday, August 27, 2024
8:00 AM - 6:00 PM CEST
Location: Convention Hall II
- SS
Sophie Scanlon, MSc (she/her/hers)
Epidemiologist
MHRA, United Kingdom - PD
Preeti Datta-Nemdharry
MHRA, United Kingdom
Presenting Author(s)
Co-Author(s)
Background: There is interest in using pharmacokinetic-pharmacodynamic (PKPD) models and an exposure-based bracketing approach to support rapid development of long-acting contraceptives. These would benefit women by improving compliance and effectiveness, reducing unintended pregnancies. This study aims to determine the value of real world data from the UK Clinical Practice Research Datalink (CPRD) in informing PKPD models by assessing the data’s utility in establishing effectiveness and safety of a hormonal contraceptive.
Objectives: To evaluate use of CPRD Aurum data in estimating effectiveness (rate of unintended pregnancy) and safety (rates of pre-specified adverse events (AEs)), of levonorgestrel (LNG) oral and implant contraceptives.
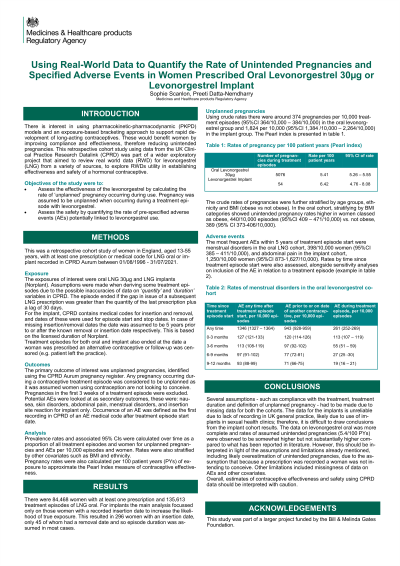
Methods: This was a retrospective cohort study of a representative sample of women in England, aged 13-55 years, with at least one prescription or medical code for LNG oral or implant recorded in CPRD between 01/08/1996 - 31/07/2021. Treatment episodes of exposures were derived based on assumptions of duration. Pregnancy rates were calculated per 100 patient years (PYs) of exposure to approximate the Pearl Index measure of contraceptive effectiveness. Prevalence rates of unintended pregnancies and possible AEs, per 10,000 episodes/women, were also calculated and stratified by covariates and time since treatment episode start.
Results: There were 84,468 women with at least one prescription and 135,613 treatment episodes of LNG oral. For implants 296 women had an insertion date, but only 45 had a removal date and so episode duration was assumed in most cases.
The Pearl index for LNG oral cohort was 5.41/100PYs (95%CI 5.26-5.55/100 PYs) and for implants was 6.42/100 PYs (95%CI 4.76-8.08/100 PYs). For the oral cohort, rates were highest in the 3 months post treatment start date 7.06/100 PYs (95%CI 6.78-7.35/100 PYs).
Stratifying the oral cohort by BMI categories showed unintended pregnancy rates higher in women classed as obese, 440/10,000 episodes (95%CI 409 – 471/10,000) vs. not obese, 389 (95% CI 373-406/10,000).
The most frequent AEs within 5 years of treatment episode start were menstrual disorders in the oral LNG cohort, 398/10,000 women (95%CI 385 – 411/10,000), and abdominal pain in the implant cohort, 1,250/10,000 women (95%CI 873-1,627/10,000).
Conclusions: When looking at rates of unintended pregnancies in CPRD data, several assumptions were made, and missingness was an issue for covariates. The data for the implants is unreliable due to lack of recording in UK general practice, likely due to use of implants in sexual health clinics; therefore, it is difficult to draw conclusions from the implant cohort results. Overall, estimates of contraceptive effectiveness and safety using CPRD data should be interpreted with caution.
Objectives: To evaluate use of CPRD Aurum data in estimating effectiveness (rate of unintended pregnancy) and safety (rates of pre-specified adverse events (AEs)), of levonorgestrel (LNG) oral and implant contraceptives.
Methods: This was a retrospective cohort study of a representative sample of women in England, aged 13-55 years, with at least one prescription or medical code for LNG oral or implant recorded in CPRD between 01/08/1996 - 31/07/2021. Treatment episodes of exposures were derived based on assumptions of duration. Pregnancy rates were calculated per 100 patient years (PYs) of exposure to approximate the Pearl Index measure of contraceptive effectiveness. Prevalence rates of unintended pregnancies and possible AEs, per 10,000 episodes/women, were also calculated and stratified by covariates and time since treatment episode start.
Results: There were 84,468 women with at least one prescription and 135,613 treatment episodes of LNG oral. For implants 296 women had an insertion date, but only 45 had a removal date and so episode duration was assumed in most cases.
The Pearl index for LNG oral cohort was 5.41/100PYs (95%CI 5.26-5.55/100 PYs) and for implants was 6.42/100 PYs (95%CI 4.76-8.08/100 PYs). For the oral cohort, rates were highest in the 3 months post treatment start date 7.06/100 PYs (95%CI 6.78-7.35/100 PYs).
Stratifying the oral cohort by BMI categories showed unintended pregnancy rates higher in women classed as obese, 440/10,000 episodes (95%CI 409 – 471/10,000) vs. not obese, 389 (95% CI 373-406/10,000).
The most frequent AEs within 5 years of treatment episode start were menstrual disorders in the oral LNG cohort, 398/10,000 women (95%CI 385 – 411/10,000), and abdominal pain in the implant cohort, 1,250/10,000 women (95%CI 873-1,627/10,000).
Conclusions: When looking at rates of unintended pregnancies in CPRD data, several assumptions were made, and missingness was an issue for covariates. The data for the implants is unreliable due to lack of recording in UK general practice, likely due to use of implants in sexual health clinics; therefore, it is difficult to draw conclusions from the implant cohort results. Overall, estimates of contraceptive effectiveness and safety using CPRD data should be interpreted with caution.
