Cancer
Session: Poster Session A
(083) Utility of Digitally-Enabled Tools in Community Education and Activation for LDCT screening for Lung Cancer
Monday, August 26, 2024
8:00 AM - 6:00 PM CEST
Location: Convention Hall II
- SH
Sutton Harris, MS (she/her/hers)
Senior Clinical Project Manager
Pluto Health, United States
Presenting Author(s)
Background: Digital technologies are an increasingly used method by which studies can speed up data gathering, and empower and benefit researchers and trial teams, although their impact in community-based activation remains to be validated.
Objectives: To activate low dose computed tomography (LDCT) for lung cancer screening through an educational initiative and to evaluate the efficacy of digital tools for longitudinal monitoring and study screening. Our team hypothesizes that by reaching out electronically with tailored education to high-risk cohorts eligible for screening, we will see an impact on screening rates and secondarily an increase in engagement between physician and patient compared to a control that receives no education. We will also explore its impact on the ability to affect health equity, provide care to disparate populations, and reduce burden on clinical teams.
Methods: This randomized controlled trial employs decentralized recruitment based on USPSTF guidelines on lung cancer screening for high-risk smokers. Participants are randomized to receipt of educational materials at enrollment, or receipt of identical materials after 12-months. Materials introduce benefits of LDCT for early detection of lung cancer and improved prognosis. Screening activation rate will be compared, and other variables will be tracked via digital tools, including physician visits, reasons for LDCT screening or healthcare services, participant reported outcomes and surveys, longitudinal outcomes, and engagement with educational materials. In addition, medical history, smoking history, smoking medications and sociodemographic information will be summarized. Participants with complete data (also an indication of the ability to follow them over time) will be summarized to show the utility of digital tools and their impact on health equity.The study at large is ongoing, however, our team hypothesizes that by reaching out electronically with tailored education to high-risk cohorts eligible for screening, we will see an impact on screening rates and secondarily an increase in engagement between physician and patient compared to a control that receives no education.
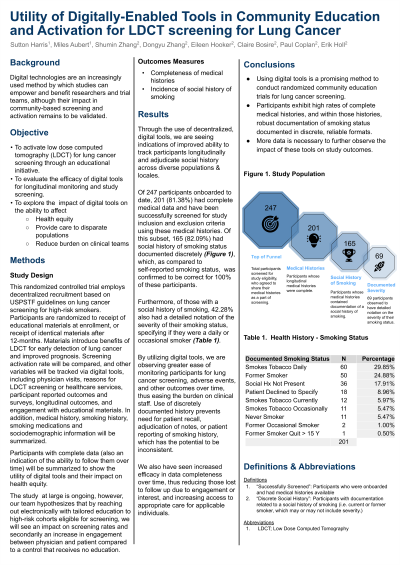
Results: Through the use of decentralized, digital tools, we are seeing indications of improved ability to track participants longitudinally and adjudicate social history across diverse populations & locales. Of 247 participants onboarded to date, 201 (81.38%) had complete medical data and have been successfully screened for study inclusion and exclusion criteria using these medical histories. Of this subset, 165 (82.09%) had social history of smoking status documented discretely, which, as compared to self-reported smoking status, was confirmed to be correct for 100% of these participants. Furthermore, of those with a social history of smoking, 42.28% also had a detailed notation of the severity of their smoking status, specifying if they were a daily or occasional smoker. By utilizing digital tools, we are observing greater ease of monitoring participants for lung cancer screening, adverse events, and other outcomes over time, thus easing the burden on clinical staff. Use of discretely documented history prevents need for patient recall, adjudication of notes, or patient reporting of smoking history, which has the potential to be inconsistent. We also have seen increased efficacy in data completeness over time, thus reducing those lost to follow up due to engagement or interest, and increasing access to appropriate care for applicable individuals.
Conclusions: Using digital tools is a promising method to conduct randomized community education trials for lung cancer screening. Participants exhibit high rates of complete medical histories, and within those histories, robust documentation of smoking status documented in discrete, reliable formats. More data is necessary to further observe the impact of these tools on study outcomes.
Objectives: To activate low dose computed tomography (LDCT) for lung cancer screening through an educational initiative and to evaluate the efficacy of digital tools for longitudinal monitoring and study screening. Our team hypothesizes that by reaching out electronically with tailored education to high-risk cohorts eligible for screening, we will see an impact on screening rates and secondarily an increase in engagement between physician and patient compared to a control that receives no education. We will also explore its impact on the ability to affect health equity, provide care to disparate populations, and reduce burden on clinical teams.
Methods: This randomized controlled trial employs decentralized recruitment based on USPSTF guidelines on lung cancer screening for high-risk smokers. Participants are randomized to receipt of educational materials at enrollment, or receipt of identical materials after 12-months. Materials introduce benefits of LDCT for early detection of lung cancer and improved prognosis. Screening activation rate will be compared, and other variables will be tracked via digital tools, including physician visits, reasons for LDCT screening or healthcare services, participant reported outcomes and surveys, longitudinal outcomes, and engagement with educational materials. In addition, medical history, smoking history, smoking medications and sociodemographic information will be summarized. Participants with complete data (also an indication of the ability to follow them over time) will be summarized to show the utility of digital tools and their impact on health equity.The study at large is ongoing, however, our team hypothesizes that by reaching out electronically with tailored education to high-risk cohorts eligible for screening, we will see an impact on screening rates and secondarily an increase in engagement between physician and patient compared to a control that receives no education.
Results: Through the use of decentralized, digital tools, we are seeing indications of improved ability to track participants longitudinally and adjudicate social history across diverse populations & locales. Of 247 participants onboarded to date, 201 (81.38%) had complete medical data and have been successfully screened for study inclusion and exclusion criteria using these medical histories. Of this subset, 165 (82.09%) had social history of smoking status documented discretely, which, as compared to self-reported smoking status, was confirmed to be correct for 100% of these participants. Furthermore, of those with a social history of smoking, 42.28% also had a detailed notation of the severity of their smoking status, specifying if they were a daily or occasional smoker. By utilizing digital tools, we are observing greater ease of monitoring participants for lung cancer screening, adverse events, and other outcomes over time, thus easing the burden on clinical staff. Use of discretely documented history prevents need for patient recall, adjudication of notes, or patient reporting of smoking history, which has the potential to be inconsistent. We also have seen increased efficacy in data completeness over time, thus reducing those lost to follow up due to engagement or interest, and increasing access to appropriate care for applicable individuals.
Conclusions: Using digital tools is a promising method to conduct randomized community education trials for lung cancer screening. Participants exhibit high rates of complete medical histories, and within those histories, robust documentation of smoking status documented in discrete, reliable formats. More data is necessary to further observe the impact of these tools on study outcomes.
