Diabetes
Session: Poster Session B
(080) Utilization of sodium-glucose cotransporter 2 inhibitors post-regulatory approval as an adjunctive therapy for type 1 diabetes mellitus: Insight from real-world experience in Japan
Tuesday, August 27, 2024
8:00 AM - 6:00 PM CEST
Location: Convention Hall II
- MT
Masato Takeuchi, MD, MPH, PhD (he/him/his)
Professor
Department of Public Health, Shizuoka Graduate University of Public Health
Shizuoka, Japan
Presenting Author(s)
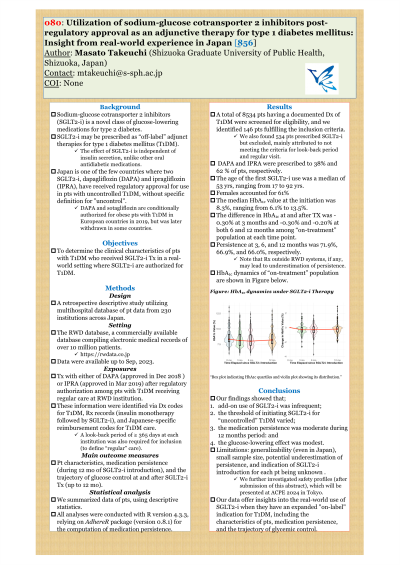
Background: Sodium-glucose cotransporter 2 (SGLT2) inhibitors may be prescribed as “off-label” adjunct therapies for type 1 diabetes mellitus (T1DM). Japan is one of the few countries where two SGLT2 inhibitors—dapagliflozin and ipragliflozin—have received regulatory approval for use in patients with uncontrolled T1DM.
Objectives: To determine the clinical characteristics of patients with T1DM who received SGLT2 inhibitor therapy in a real-world setting.
Methods: We analyzed data from the RWD database, a multihospital database that contains patient data from 230 institutions across Japan. We selected patients with T1DM who initiated treatment with either dapagliflozin or ipragliflozin after regulatory approval, with regular care for T1DM at medical institutions participating in the RWD database; this information was identified via diagnostic codes for T1DM, prescription records (insulin monotherapy followed by SGLT2 inhibitors), and Japanese-specific reimbursement codes for T1DM. Patient characteristics, medication persistence, and the trajectory of glucose control before and after treatment were investigated.
Results: We screened over 20 million individuals who had at least one medical contact with the institutions in the RWD database. From 8534 patients with a documented diagnosis of T1DM, we identified 101 patients who met the inclusion criteria. The median age at SGLT2 inhibitor initiation was 51 years, and 56% of the patients were females. Dapagliflozin and ipragliflozin were used almost equally. The mean hemoglobin A1c (HbA1c) value over the preceding 12 months was 8.4%, ranging from 6.0% to 11.6%. The medication persistence at 3, 6 and 12 months was 97%, 93%, and 89%, respectively. The difference in HbA1c before and after treatment was -0.39% at 3 months and -0.26% at both 6 and 12 months.
Conclusions: Despite the limited sample size, our data offer insights into the real-world use of SGLT2 inhibitors when they have an expanded "on-label" indication for T1DM. Future research that includes an adverse event profile of those treated with such SGLT2 inhibitors are warranted.
Objectives: To determine the clinical characteristics of patients with T1DM who received SGLT2 inhibitor therapy in a real-world setting.
Methods: We analyzed data from the RWD database, a multihospital database that contains patient data from 230 institutions across Japan. We selected patients with T1DM who initiated treatment with either dapagliflozin or ipragliflozin after regulatory approval, with regular care for T1DM at medical institutions participating in the RWD database; this information was identified via diagnostic codes for T1DM, prescription records (insulin monotherapy followed by SGLT2 inhibitors), and Japanese-specific reimbursement codes for T1DM. Patient characteristics, medication persistence, and the trajectory of glucose control before and after treatment were investigated.
Results: We screened over 20 million individuals who had at least one medical contact with the institutions in the RWD database. From 8534 patients with a documented diagnosis of T1DM, we identified 101 patients who met the inclusion criteria. The median age at SGLT2 inhibitor initiation was 51 years, and 56% of the patients were females. Dapagliflozin and ipragliflozin were used almost equally. The mean hemoglobin A1c (HbA1c) value over the preceding 12 months was 8.4%, ranging from 6.0% to 11.6%. The medication persistence at 3, 6 and 12 months was 97%, 93%, and 89%, respectively. The difference in HbA1c before and after treatment was -0.39% at 3 months and -0.26% at both 6 and 12 months.
Conclusions: Despite the limited sample size, our data offer insights into the real-world use of SGLT2 inhibitors when they have an expanded "on-label" indication for T1DM. Future research that includes an adverse event profile of those treated with such SGLT2 inhibitors are warranted.
